Molina Medication Prior Authorization Form
Molina Medication Prior Authorization Form - Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Web drug prior authorization form michigan medicaid and marketplace phone: Progress notes cholesterol lowering (ie. Edit, sign and save prior authorization req form. ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. Web the preferred drug list and the pdl criteria guide can be found here. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. The forms are also available on the frequently used forms page. Web prior authorization lookup tool.
Please enter one email address * email this article to: The forms are also available on the frequently used forms page. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Progress notes cholesterol lowering (ie. Web prior authorization lookup tool. Web the preferred drug list and the pdl criteria guide can be found here. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Items on this list will only be dispensed after prior authorization from molina healthcare.
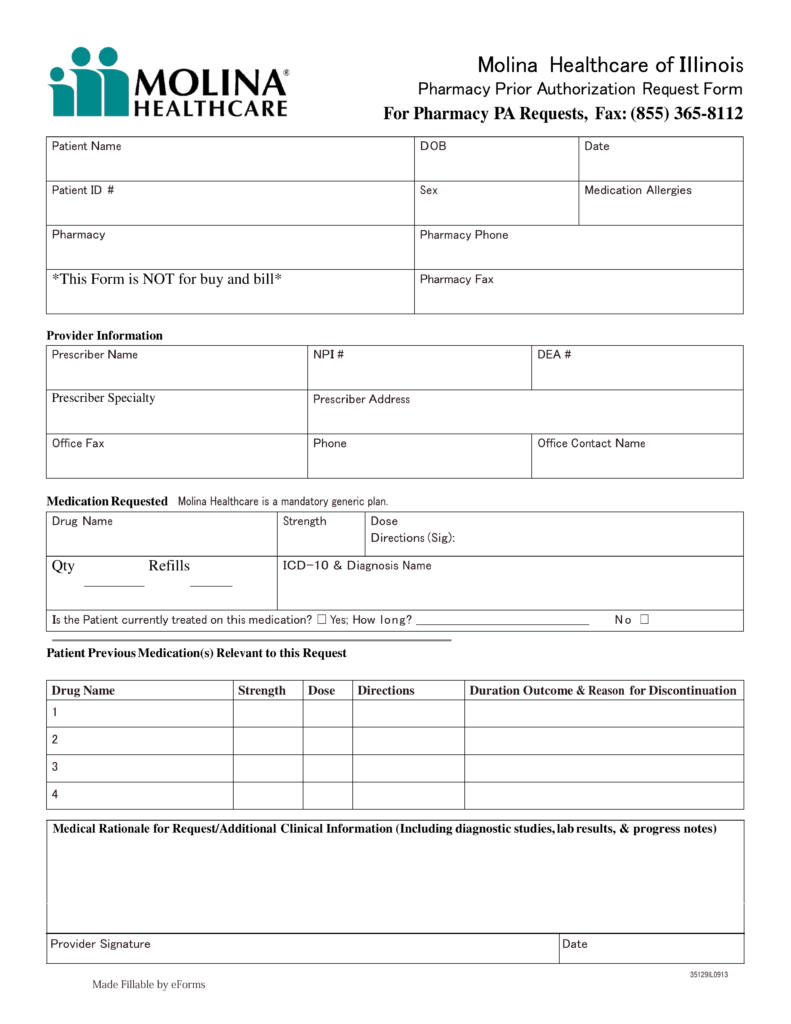
Please see the clinical pa criteria that molina has implemented below. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Web drug prior authorization form michigan medicaid and marketplace phone: Web the preferred drug list and the pdl criteria guide can be found here. Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax: Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web prior authorization lookup tool. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for.
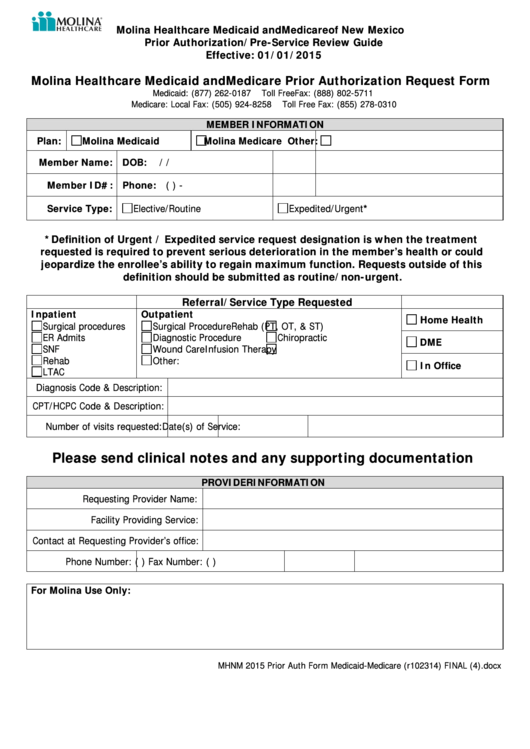
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Please enter one email address * email this article to: Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax: Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Progress notes cholesterol lowering (ie. ☐ new request ☐ reauthorization patient previous medication(s).
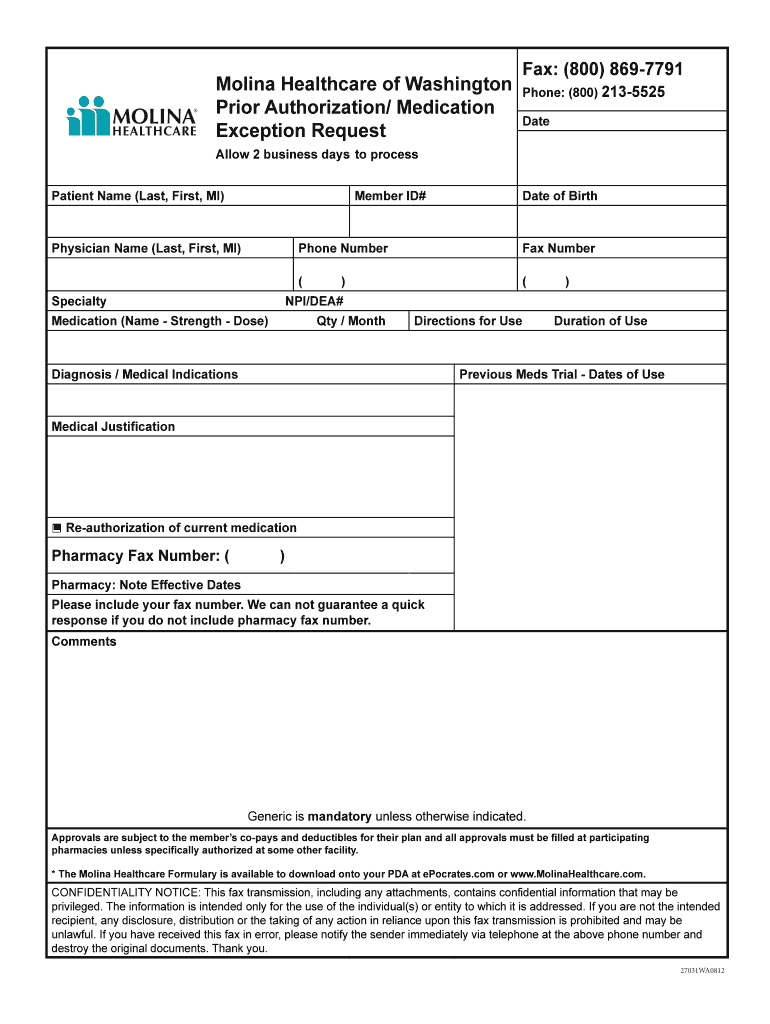
Molina Healthcare Medication Prior Authorization/Exceptions Request
Please enter one email address * email this article to: It is needed before you can get certain services or drugs. The forms are also available on the frequently used forms page. Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Web the preferred drug list and the pdl criteria guide can be found here.
Prior Authorization Form For Molina Medicare Universal Network
Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Please enter one email address * email this article to: Pharmacy prior authorization forms ; Items on this list will only be dispensed after prior authorization from molina healthcare. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s.
Molina Medicare Medication Prior Authorization Form Form Resume
Pdffiller allows users to edit, sign, fill & share all type of documents online. Web prior authorization lookup tool. Please see the clinical pa criteria that molina has implemented below. It is needed before you can get certain services or drugs. Progress notes cholesterol lowering (ie.
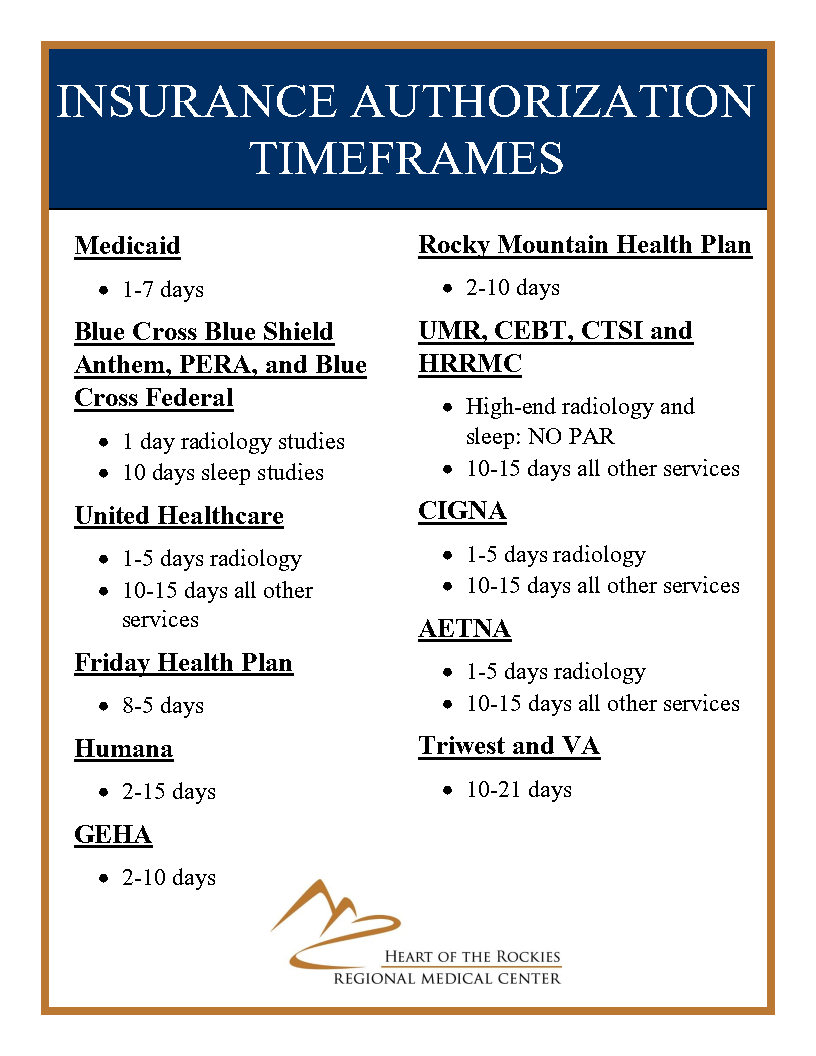
Insurance Prior Authorization Timeframes Medical Center in Salida
Pdffiller allows users to edit, sign, fill & share all type of documents online. Please see the clinical pa criteria that molina has implemented below. Web prior authorization lookup tool. Web the preferred drug list and the pdl criteria guide can be found here. Formulary drugs (formulary drug search here ) may require a clinical prior authorization.
Molina Authorization Form Fill Online, Printable, Fillable, Blank
Edit, sign and save prior authorization req form. Web prior authorization lookup tool. Items on this list will only be dispensed after prior authorization from molina healthcare. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Web drug prior authorization form michigan medicaid and marketplace phone:
Molina Medicare Medication Prior Authorization Form Form Resume
Molina healthcare prior authorization request form and instructions. Please see the clinical pa criteria that molina has implemented below. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Pdffiller allows users to edit, sign, fill & share all type of documents online. Progress notes.
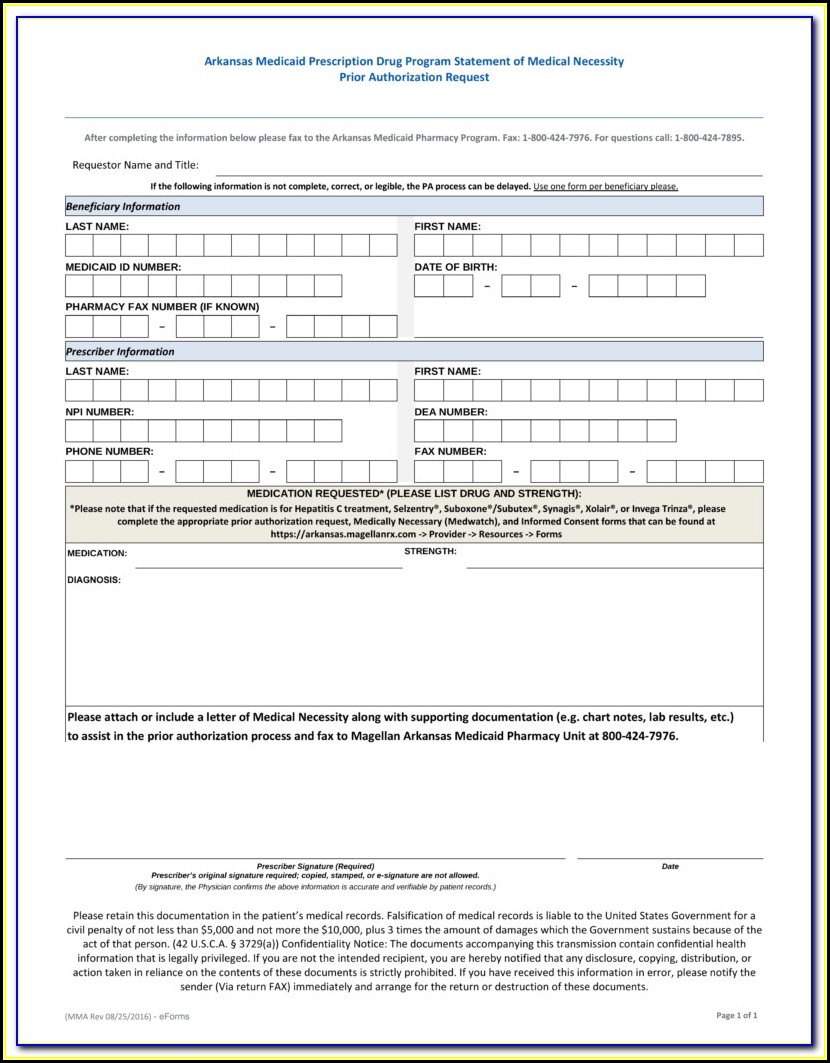
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Web drug prior authorization form michigan medicaid and marketplace phone: ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. Please see the clinical pa criteria that molina has implemented below. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior..
UT Molina Healthcare Prior Authorization Form 20162022 Fill and Sign
Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax: Pdffiller allows users to edit, sign, fill & share all type of documents online. Progress notes cholesterol lowering (ie. Formulary drugs (formulary drug search here ).
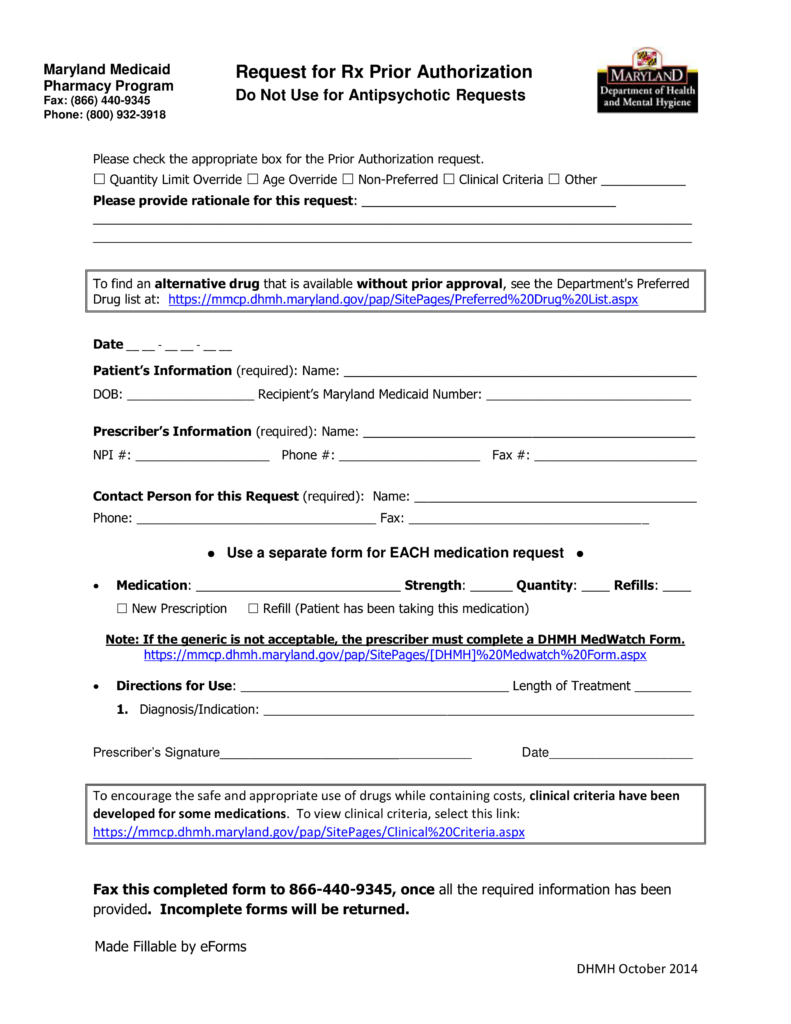
Free Maryland Medicaid Prior (Rx) Authorization Form PDF eForms
Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Edit, sign and save prior authorization req form. Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests,.
Pharmacy Prior Authorization Forms ;
Molina healthcare prior authorization request form and instructions. Please enter one email address * email this article to: Progress notes cholesterol lowering (ie. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations?
Edit, Sign And Save Prior Authorization Req Form.
Items on this list will only be dispensed after prior authorization from molina healthcare. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit.
Web Molina Healthcare Of Illinois Pharmacy Prior Authorization Request Form For Pharmacy Pa Requests, Fax:
Web drug prior authorization form michigan medicaid and marketplace phone: It is needed before you can get certain services or drugs. Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Web prior authorization lookup tool.
The Forms Are Also Available On The Frequently Used Forms Page.
Please see the clinical pa criteria that molina has implemented below. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web the preferred drug list and the pdl criteria guide can be found here. Pdffiller allows users to edit, sign, fill & share all type of documents online.